|
Despite decades of treatments to lower cholesterol, regulate heart rhythms, and reduce salt and fat, cardiovascular disease is still the number one killer of adults in the industrialized world. It has been associated with nearly 300 independent risk factors, among them high LDL, low HDL, male gender, smoking, obesity, insulin resistance, sedentary lifestyle, age, and hypertension. Blood viscosity is the common factor ties all these factors together.
Blood viscosity – a measurement of the thickness and stickiness of an individual's blood – is associated with each of those risk factors, either as a contributor or an effect. Understanding blood viscosity and how it contributes to the development of atherosclerotic plaques and thrombosis, how to test for it, and how to treat it are essential to our practices as primary care physicians. There are effective natural treatments that can alter blood viscosity safely, preserving health and potentially saving lives.
The Physics of Blood Viscosity
To understand blood viscosity and how it affects the arterial walls, it is useful to understand the physics involved in fluids. Blood is not the same thickness and stickiness – or viscosity – at all times. While water is no thicker in a still pond than in a fast-running stream, blood actually thickens as it slows down. During diastole, slower-moving red blood cells cling together more easily and can even form rouleaux, structures that look like stacks of coins under a microscope. These clinging red blood cells make the blood more viscous. During slow flow, aggregation of platelets and intermolecular reactions between plasma and cellular components further contribute to increasing viscosity. At the other end of the cardiac cycle – systole – blood flows more rapidly, resulting in dispersion of blood components and decreased viscosity. Therefore, blood viscosity fluctuates with every heartbeat, from lesser to greater and back. Blood at diastole can be anywhere from 5 to 20 times as viscous as the same blood at systole. However, even blood at systole can be more viscous than optimal, and this plays an important role in the development of atherosclerotic plaques.
High iron levels have been thought to be a key factor in plaque development, but if that were the case, one would expect to see atherosclerotic plaques developing uniformly throughout the body. The effect of blood viscosity explains why atherosclerotic plaques are found almost exclusively at the bifurcations of large arteries in the neck, around the heart, and in the large arteries of the legs. These bifurcations create "eddies," places where the blood becomes turbulent. During systole, the walls of the large vessels nearest the heart are subjected to the force of blood propelled under high shear, or pressure. Blood viscosity thus determines not only how hard the heart has to work to circulate the blood, but also the level of physical injury that the blood can cause to the inner walls of the arteries. Viscous blood has an abrasive quality that damages the endothelium during these high-shear assaults, leading to inflammation. Plaques are formed to protect these delicate areas from the constant battering of erosive, viscous blood. Plaques also form in bifurcations of the large arteries of the legs, where the blood is subject to increased shear due to the effects of gravity.
Factors Affecting Blood Viscosity
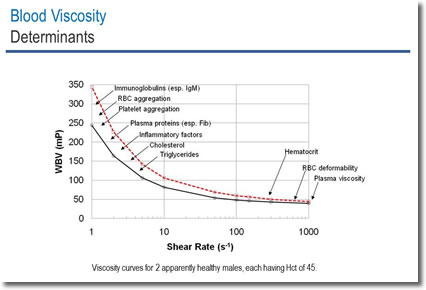
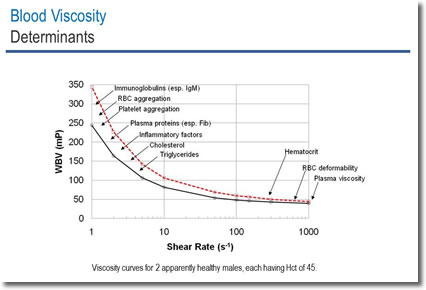
Blood viscosity is determined directly by four primary factors: hematocrit, RBC (red blood cell) deformability, plasma viscosity, and RBC sedimentation/aggregation. The effect of hematocrit makes intuitive sense – the more blood cells that one has, the thicker one's blood is going to be. Hematocrit is responsible for about 50% of the total contribution of these four factors to blood viscosity.
Not as obvious is the role of erythrocyte deformability. This refers to the ability of RBCs to bend and fold themselves in order to make their way through the slender passageways of the capillaries. RBC deformability is inversely correlated with blood viscosity, meaning that the more deformable the RBCs are, the less viscous the blood. Young RBCs are more deformable than older RBCs. Erythrocyte deformability is, after hematocrit, the second most important determinant of blood viscosity.
Plasma viscosity refers to the viscosity of the noncellular matrix of the blood. An important determinant of plasma viscosity is hydration status, and there are many others. Research published in the journal Aviation, Space, and Environmental Medicine demonstrated that dehydration increases systolic blood viscosity by 9.3% and diastolic blood viscosity by 12.5%.
RBC sedimentation/aggregation is the tendency of RBCs to be attracted to each other and stick together. There are numerous factors that can increase sedimentation and aggregation. Blood viscosity correlates directly with both RBC aggregation and plasma viscosity.
The rest of the nearly 300 risk factors for cardiovascular disease are correlated with blood viscosity, either by affecting one of the four primary determinants, or because increased blood viscosity is a contributing cause of the condition. For example, high triglycerides increase the viscosity of the plasma; inflammation increases cytokines that affect the polarity of RBCs, making them stickier and more attracted to each other. On the other hand, cognitive decline and migraines do not cause higher blood viscosity, but they are correlated with it because elevated blood viscosity contributes to these conditions.
Differences Between Men and Women
It is well established that men of any age are at higher risk for cardiovascular events than premenopausal women. The fact that a woman's risk increases significantly after menopause has been thought to be due to decreasing levels of estrogen with concomitant loss of its protective effects. Studies show that women who have had hysterectomies (surgical menopause) are at increased risk for cardiovascular disease – regardless of whether they kept their ovaries. Even younger women who have had hysterectomies and retained their ovaries and thus have no change in estrogen status are still at increased risk. Why is that?
Remember the four primary determinants of blood viscosity: hematocrit, RBC deformability, RBC aggregation, and plasma viscosity. All four are highly affected by a woman's monthly blood loss. The effect on hematocrit is obvious. RBC deformability may be less so. RBCs have a lifespan of about 100 to 120 days. Young RBCs are more flexible and deformable than older ones. Because of monthly bleeding, a woman makes more new blood cells than a man. Her blood contains about 80% more young blood cells than a man's and about 85% fewer old blood cells. Older RBCs are also more likely aggregate than are younger RBCs. In addition, they are more fragile than younger cells and more likely to break apart, releasing hemoglobin into the plasma. Plasma free hemoglobin binds nitric oxide, reducing the ability of NO to perform its functions as a vasodilator and an inhibitor of platelet aggregation.
Delivery of O2 to the Tissues is Mediated by Blood Viscosity
The capacity of blood to carry oxygen to the tissues is directly correlated with hematocrit. However, it is also inversely correlated to blood viscosity. The relationship of these two parameters is expressed as the oxygen delivery index (ODI). Within the limits of normal hematocrit values for men and women, improved ODI is associated with lower hematocrit levels. So a woman with a normal hematocrit actually has a greater ability to deliver O2 to cells than a man with a higher, but normal, hematocrit. Which gives pause, when considering the use of erythropoietin both medically and in sports to improve O2 carrying capacity. It may be that we are actually decreasing O2 carrying capacity by increasing hematocrit and thereby increasing viscosity. Given the universal importance of oxygen delivery to the tissues, the relevance of blood viscosity to health maintenance and promotion is clear.
Blood Viscosity and Cardiovascular Disease
A growing number of studies point to blood viscosity's role in cardiovascular diseases. In the 1990s, the Edinburgh Artery Study observed 4860 men between ages 45 and 59 for five years and showed that the 20% of individuals with the highest viscosity had 55% of the major cardiovascular events. Only 4% of those with low viscosity had any significant cardiovascular event. The difference in mean whole blood viscosity between the two groups of patients was statistically very significant (p = 0.0003). The relationship of blood viscosity to the occurrence of cardiovascular events was at least as strong as for diastolic blood pressure and LDL cholesterol and stronger than that of smoking. These results suggest that blood viscosity is an important predictor of cardiovascular events in the adult population.
Three important studies have helped to establish the relationship between blood pressure and blood viscosity. The earliest study observed 49 normal subjects and 49 patients with untreated essential hypertension and showed a direct correlation between BP and blood viscosity among both normotensive and hypertensive subjects (p < 0.001). Systolic blood viscosity was 8% to 10% higher and diastolic blood viscosity was 16% to 28% higher in hypertensive patients compared with normotensive controls.
The Edinburgh Artery Study demonstrated that systolic BP correlated to blood viscosity in males (p < 0.001), and diastolic BP correlated to blood viscosity in both sexes (p < 0.001). Hematocrit-corrected blood viscosity levels were also significantly related to systolic and diastolic BP in both sexes.
A third study followed 331 men newly diagnosed with essential hypertension for up to 12 years. Patients were grouped into three categories by their diastolic blood viscosity levels: high, medium, and low. The highest tertile for diastolic viscosity were more than three times as likely to have cardiovascular events than the lowest diastolic viscosity tertile, even though all the men were hypertensive (hazard ratio = 3.42, p = 0.006).
Blood Viscosity and Diabetes
It is has been demonstrated by many investigators that diabetics have elevated blood viscosity. It is also known that red cell deformability and the osmolarity of the blood – both affected by uncontrolled blood glucose – mediate blood viscosity changes and the onset of small vessel disease. Diabetics have a higher proportion of red cells that are relatively nondeformable and which must pass through relatively long, narrow capillaries to deliver O2 and nutrients to cells. Capillaries can be smaller than erythrocyte diameter, resulting in injuries to the capillary walls. This injury is dramatically increased as erythrocyte deformability is impaired. Blindness, kidney insufficiency, and leg ischemia are the first comorbidities to appear because the associated organs are the most dependent on microperfusion for function.
Blood Viscosity and Cognitive Decline
Multiple forms of cognitive decline, including dementia and Alzheimer's disease, are affected by increased blood viscosity. In a 2010 report of the Edinburgh Artery Study, blood viscosity was shown to predict cognitive decline over a four-year period in 452 elderly subjects (p < 0.05). Blood viscosity is an important determinant of the circulatory flow of blood and was shown to be significantly linked with cognitive function.
Other Conditions Associated with Elevated Blood Viscosity
Increased blood viscosity is associated with a surprising range of conditions. In women who develop preeclampsia in pregnancy, blood viscosity increases sharply about six weeks before clinical symptoms develop. Increased blood viscosity is also associated with cesarean sections due to fetal distress and with fetal demise. Retinal vein occlusion and glaucoma are associated with increased blood viscosity. Dr. Kenneth R. Kensey, a prominent researcher in the field, went so far as to say that all ophthalmological pathologies can be traced to elevated blood viscosity. Other conditions that have been linked to blood viscosity include diabetes, migraines, Reynaud's syndrome, gout, cirrhosis, and rheumatoid arthritis.
Testing for Blood Viscosity
There are three kinds of testing for blood viscosity. Serum or plasma viscosity is a single measurement with a narrow clinical utility that does not account for hematocrit, blood cell deformability, or factors increasing RBC aggregation. Whole blood viscosity, available from a few reference labs, does include these contributing factors. WBV is generally done using a Brookfield viscometer, an older technology designed for measuring the viscosity of house paint or engine oil. It yields a single measurement that is roughly equivalent to the viscosity of the blood at systolic pressures, when it is the most fluid and the least sticky.
The newest and most advanced testing uses a Hemathix SCV-200 automated scanning capillary tube viscometer (formerly known as the Rheolog), which is capable of measuring viscosity over the complete range of physiologic values experienced in a cardiac cycle (10,000 shear rates) with a single continuous measurement. While there are several of the Hemathix viscometers in use in research settings, there is at this time only one commercial laboratory using the Hemathix for blood viscosity testing.
Blood viscosity rises and falls from one extreme to the other with every cardiac cycle – much like blood pressure. Like blood pressure, a meaningful blood viscosity test requires two numbers: systolic blood viscosity and diastolic blood viscosity. Systolic blood viscosity is affected by hematocrit and plasma viscosity and is highly affected by hydration status. Diastolic viscosity is affected by numerous factors, including the stickiness of platelets, immune complexes that increase the aggregation of RBCs, triglycerides, cholesterol, and many more. Blood viscosity testing that measures only a single (systolic) shear rate misses the impact of these factors and thus has significantly less clinical utility.
Tracking Blood Viscosity to Improve Patient Outcomes
Integrative practitioners are already employing many of the natural therapeutics and lifestyle changes that contribute to a lowered blood viscosity, and seeing improved outcomes in their patients. Blood viscosity testing can be used to screen patients who may be at risk and to document the effectiveness of our treatments. We also see a growing usefulness of this test in research for directly monitoring the efficacy of treatments intended to improve circulation and perfusion.
Blood viscosity testing is indicated for any patient with a personal or family history of heart disease, stroke, hypertension, or diabetes; for women with a history of taking oral contraceptives, especially those designed to decrease the frequency of menstrual periods; for women who have had a hysterectomy, have irregular periods, or are menopausal; patients with ocular disorders such as macular degeneration or glaucoma; women with a history of pregnancy-induced hypertension or preeclampsia, especially those who are currently pregnant; patients with signs of decreasing cognitive function; and the list goes on, as tissue perfusion and therefore optimal blood viscosity is fundamental to cellular health and regeneration across the board.

 Dr. Pushpa Larsen graduated from Bastyr University with a doctorate in naturopathic medicine and certificates in naturopathic midwifery and spirituality, health and medicine. She has worked as a research clinician for the Bastyr University Research Institute and as affiliate clinical faculty for Bastyr University, training students in her clinic. She was in private practice in Seattle for 10 years before joining Meridian Valley Lab as a consulting physician, and maintains a small private practice primarily focused on bioidentical hormone therapy. She consults with hundreds of doctors every year on the use and interpretation of 24-hour urine hormone profiles, as well as other tests offered by Meridian Valley Lab. She has previously published and presented on the use of carotid intima-media thickness (CIMT) scanning in primary-care settings for early detection of cardiovascular disease. She can be reached at plarsen@meridianvalleylab.com or at 425-271-8689. Dr. Pushpa Larsen graduated from Bastyr University with a doctorate in naturopathic medicine and certificates in naturopathic midwifery and spirituality, health and medicine. She has worked as a research clinician for the Bastyr University Research Institute and as affiliate clinical faculty for Bastyr University, training students in her clinic. She was in private practice in Seattle for 10 years before joining Meridian Valley Lab as a consulting physician, and maintains a small private practice primarily focused on bioidentical hormone therapy. She consults with hundreds of doctors every year on the use and interpretation of 24-hour urine hormone profiles, as well as other tests offered by Meridian Valley Lab. She has previously published and presented on the use of carotid intima-media thickness (CIMT) scanning in primary-care settings for early detection of cardiovascular disease. She can be reached at plarsen@meridianvalleylab.com or at 425-271-8689.
 Ralph E. Holsworth Jr. received his doctor of osteopathy from the University of Health Sciences, College of Osteopathic Medicine, Kansas City, Missouri. He is a board-certified osteopathic family physician previously serving rural and underserved regions of New Mexico and Colorado in clinic practice and as an emergency room attending physician. He currently sees patients at the Tahoma Clinic in Renton, Washington, where he takes a special interest in cardiovascular conditions. He has been doing research in the field of blood viscosity for several years and is a consultant to Meridian Valley Lab on the development of cutting-edge blood viscosity testing. In addition to the above positions, Dr. Holsworth is a member of the editorial board for the Journal of Applied Clinical Thrombosis and Hemostasis and the Japan Nattokinase Research Association. He has been involved in clinical research with oral systemic enzymes as an adjuvant in cancer treatment and has authored several publications related to antioxidant properties of electrolyzed water and nattokinase, a fibrinolytic enzyme. Ralph E. Holsworth Jr. received his doctor of osteopathy from the University of Health Sciences, College of Osteopathic Medicine, Kansas City, Missouri. He is a board-certified osteopathic family physician previously serving rural and underserved regions of New Mexico and Colorado in clinic practice and as an emergency room attending physician. He currently sees patients at the Tahoma Clinic in Renton, Washington, where he takes a special interest in cardiovascular conditions. He has been doing research in the field of blood viscosity for several years and is a consultant to Meridian Valley Lab on the development of cutting-edge blood viscosity testing. In addition to the above positions, Dr. Holsworth is a member of the editorial board for the Journal of Applied Clinical Thrombosis and Hemostasis and the Japan Nattokinase Research Association. He has been involved in clinical research with oral systemic enzymes as an adjuvant in cancer treatment and has authored several publications related to antioxidant properties of electrolyzed water and nattokinase, a fibrinolytic enzyme.

Notes
1. Kensey KR, Cho Y. Physical principles and circulation: hemodynamics. In: The Origin of Atherosclerosis: What Really Initiates the Inflammatory Process. 2nd ed. Summersville, WV: SegMedica; 2007:33–50.
2. Sloop GD. A unifying theory of atherogenesis. Med Hypotheses. 1996; 47:321–325.
3. Doi T et al. Plasma volume and blood viscosity during 4 h sitting in a dry environment. Aviat Space Environ Med. 2004;75(6):500–504.
4. Fowkes FG, Pell JP, et al. Sex differences in susceptibility to etiologic factors for peripheral atherosclerosis. Importance of plasma fibrinogen and blood viscosity. Arterioscler Thromb 1994;14:862–868.
5. Kamaneva MV, Watach MJ, Borovetz HS. Gender difference in rheologic properties of blood and risk of cardiovascular diseases. Clin Hemorheol Microcirc. 1999, 21:357–363
6. Sloop GD, Garber DW. The effects of low-density lipoprotein and high-density lipoprotein on blood viscosity correlate with their association with risk of atherosclerosis in humans. Clin Sci. 1997;92:473–479.
7. Lowe GD. Blood viscosity, lipoproteins, and cardiovascular risk. Circulation 1992;85:2329–2331.
8. de Simone G, Devereux RB, Chien S, et al. Relation of blood viscosity to demographic and physiologic variables and to cardiovascular risk factors in apparently normal adults. Circulation 1990;81:107–117.
9. Lowe GD, Lee AJ, Rumley A, et al. Blood viscosity and risk of cardiovascular events: the Edinburgh Artery Study. Br J Haematol 1997; 96:168–173.
10. Letcher RL, Chien S, et al. Direct relationship between blood pressure and blood viscosity in normal and hypertensive subjects. Role of fibrinogen and concentration. Am J Med. 1981;70:1195–1202.
11. Fowkes FG, Lowe GD, et al. The relationship between blood viscosity and blood pressure in a random sample of the population aged 55 to 74 years. Eur Heart J. 1993;14:597–601.
12. Ciuffetti G, Schillaci G, et al. Prognostic impact of low-shear whole blood viscosity in hypertensive men. Eur J Clin Invest. 2005;35:93–98.
13. Tamariz LJ, Young JH, Pankow JS, et al. Blood viscosity and hematocrit as risk factors for type 2 diabetes mellitus: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Epidemiol. 2008; 168:1153–1160.
14. Jax TW, Peters AJ, Plehn G, Schoebel FC. Hemostatic risk factors in patients with coronary artery disease and type 2 diabetes - a two year follow-up of 243 patients. Cardiovasc Diabetol 2009; 8:48.
15. Rafnsson S, Deary IJ, Whiteman MC, Rumley A, Lowe GD, Fowkes FG. Haemorheological predictors of cognitive decline: the Edinburgh Artery Study. Age Ageing. 2010;39:217–222.


|
|



![]()
![]()

 Dr. Pushpa Larsen graduated from Bastyr University with a doctorate in naturopathic medicine and certificates in naturopathic midwifery and spirituality, health and medicine. She has worked as a research clinician for the Bastyr University Research Institute and as affiliate clinical faculty for Bastyr University, training students in her clinic. She was in private practice in Seattle for 10 years before joining Meridian Valley Lab as a consulting physician, and maintains a small private practice primarily focused on bioidentical hormone therapy. She consults with hundreds of doctors every year on the use and interpretation of 24-hour urine hormone profiles, as well as other tests offered by Meridian Valley Lab. She has previously published and presented on the use of carotid intima-media thickness (CIMT) scanning in primary-care settings for early detection of cardiovascular disease. She can be reached at
Dr. Pushpa Larsen graduated from Bastyr University with a doctorate in naturopathic medicine and certificates in naturopathic midwifery and spirituality, health and medicine. She has worked as a research clinician for the Bastyr University Research Institute and as affiliate clinical faculty for Bastyr University, training students in her clinic. She was in private practice in Seattle for 10 years before joining Meridian Valley Lab as a consulting physician, and maintains a small private practice primarily focused on bioidentical hormone therapy. She consults with hundreds of doctors every year on the use and interpretation of 24-hour urine hormone profiles, as well as other tests offered by Meridian Valley Lab. She has previously published and presented on the use of carotid intima-media thickness (CIMT) scanning in primary-care settings for early detection of cardiovascular disease. She can be reached at  Ralph E. Holsworth Jr. received his doctor of osteopathy from the University of Health Sciences, College of Osteopathic Medicine, Kansas City, Missouri. He is a board-certified osteopathic family physician previously serving rural and underserved regions of New Mexico and Colorado in clinic practice and as an emergency room attending physician. He currently sees patients at the Tahoma Clinic in Renton, Washington, where he takes a special interest in cardiovascular conditions. He has been doing research in the field of blood viscosity for several years and is a consultant to Meridian Valley Lab on the development of cutting-edge blood viscosity testing. In addition to the above positions, Dr. Holsworth is a member of the editorial board for the
Ralph E. Holsworth Jr. received his doctor of osteopathy from the University of Health Sciences, College of Osteopathic Medicine, Kansas City, Missouri. He is a board-certified osteopathic family physician previously serving rural and underserved regions of New Mexico and Colorado in clinic practice and as an emergency room attending physician. He currently sees patients at the Tahoma Clinic in Renton, Washington, where he takes a special interest in cardiovascular conditions. He has been doing research in the field of blood viscosity for several years and is a consultant to Meridian Valley Lab on the development of cutting-edge blood viscosity testing. In addition to the above positions, Dr. Holsworth is a member of the editorial board for the 