|
In clinical practice, practitioners often overlook the delicate interplay between the immune and nervous systems. Since these systems are intertwined and together have a significant impact on overall health and well-being, it is vital to understand how they interact.
The nervous and immune systems use neurotransmitters as chemical messengers to maintain a constant "crosstalk." More than simply markers of nervous system function, neurotransmitters govern communication throughout the body, facilitating communication between neurons, which in turn affects every cell, tissue, and system in the body. As such, they connect to immune responses and conditions in complementary and powerful ways.
For example, after undergoing urinary neurotransmitter testing through a specialty reference laboratory such as Pharmasan Labs, patients with conditions such as depression or anxiety are often found to have not only neurotransmitter imbalances, but also elevated levels of cytokines. In the same way, patients showing signs of chronic inflammation, autoimmune disease, and chronic infection are more likely to report experiencing depression, fatigue, anxiety, and insomnia.
Immune upregulation and excessive cytokine production can lead to clinical symptoms and conditions referred to as "sickness behaviors." Symptoms of sickness behavior include fatigue, difficulty concentrating, sleep disruption, anxiety, and depression. These symptoms often accompany known immunological conditions such as autoimmune disorders.
It's generally recognized that sickness behaviors result from inflammation and the immune system's increased production of cytokines. But practitioners should also consider the role played by the nervous system, since cytokine activity can influence neurotransmitter production, and neurotransmitter production can influence cytokine activity.
The Immune System Affects the Nervous System
Pro-inflammatory cytokines are produced in response to immune challenges and can have a profound effect on neurotransmitter production and function.1 Serotonin regulation and production are a good illustration of this concept. Patient complaints such as depression, anxiety, and sleep issues can be related to serotonin levels.
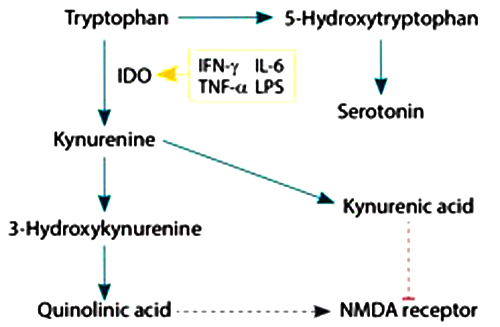
What is not so obvious is that serotonin is also affected by inflammation. Serotonin levels decrease in individuals with a chronic inflammatory condition, due in part to the shunting of tryptophan down the kynurenine pathway (Figure 1).1
Figure 1
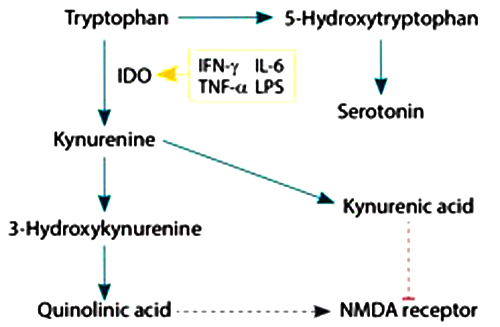
Activation of certain cytokines (such as IL-6, IFN-g, TNF-a, and LPS) can lead to activation of indoleamine 2, 3-dioxygenase (IDO), which shunts tryptophan down the kynurenine and quinolinic acid pathways, resulting in suboptimal serotonin levels.2
In addition to decreasing serotonin levels, the shunting of tryptophan down the kynurenine pathway creates other potential problems. Kynurenine metabolites have negative effects on the brain, such as oxidative stress and neurodegeneration of certain regions, both of which have been associated with conditions such as depression.3
The kynurenine pathway also affects glutamate levels. Glutamate is released upon overactivation of the kynurenine pathway by quinolinic acid (a glutamate receptor agonist) and is also implicated in depression.4 In high quantities, glutamate is excitotoxic in nature, meaning that increased levels from acute and chronic inflammatory responses could damage neurons. These examples illustrate the importance of considering the immune response as part of root cause analysis when treating patients with abnormal neurotransmitter values or psychiatric issues.
The Nervous System Affects the Immune System
Just as the immune system can affect neurotransmitters, neurotransmitters can affect the immune system. For example, norepinephrine can suppress the expression of certain pro-inflammatory cytokines, as well as increase the expression of anti-inflammatory cytokines.5
Acetylcholine is another neurotransmitter that is associated with the immune system. Acetylcholine has anti-inflammatory effects and regulates the reaction of the immune system to challenges. This regulation is important because an overly active immune system and increased cytokine levels can lead to sickness behavior and damage overall health. Increased cytokine production may also have a role in disease progression.6
Acetylcholine affects the release of other neurotransmitters such as norepinephrine. More specifically, acetylcholine binds to receptors that cause an increase in vagal nerve activity, activating the splenic nerve, which in turn causes the release of norepinephrine. Norepinephrine, as discussed above, decreases the production of certain pro-inflammatory cytokines. In addition, certain T cells produce acetylcholine as a way to control innate immune responses and inflammation.7
Testing Biomarkers Helps Customize Patient Care
These interactions between neurotransmitters and the immune system demonstrate the close linkage between the nervous and immune systems and the importance of assessing a patient's entire clinical picture. The connection between the nervous and immune systems is not always obvious, but vital to consider when evaluating patient symptoms. Getting to the root cause is the only way to restore balance and health.
Assessing neurotransmitter levels in patients with chronic inflammation, autoimmune diseases, or chronic infections can address the root causes of symptoms and provide the required data for assessing underlying imbalances. Likewise, properly identifying immune challenges and reducing chronic inflammation should be part of a comprehensive strategy for treating patients suffering from sickness behaviors such as depression, fatigue, anxiety, or insomnia.
Testing a patient's biomarkers – specifically neurotransmitter levels – can improve diagnostic accuracy and increase care effectiveness. Testing neurotransmitters can locate imbalances throughout the body. Once practitioners know a patient's key biomarkers, they can better assess the underlying health condition and personalize that patient's care.
Today's complex and recurring conditions require an approach that takes into account the interconnectedness of the nervous and immune systems. Neurotransmitter testing helps clinicians uncover adrenal and immune issues that affect proper neural balance and overall health.
Notes
1. Dantzer R, O'Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9:46–56.
2. Maes M, Leonard BE, Myint AM, Kubera M, Verkerk R.The new '5-HT' hypothesis of depression: cell-mediated immune activation induces indoleamine 2,3-dioxygenase, which leads to lower plasma tryptophan and an increased synthesis of detrimental tryptophan catabolites (TRYCATs), both of which contribute to the onset of depression. Prog Neuropsychopharmacol Biol Psychiatry. 2011 Apr 29;35(3):702–721.
3. Wichers MC, Maes M. The role of indoleamine 2,3-dioxygenase (IDO) in the pathophysiology of interferon-a-induced depression. J Psychiatry Neurosci. 2004 January;29(1):11–17.
4. Steiner J, Walter M, Gos T, et al. Severe depression is associated with increased microglial quiolinic acid in subregions of the anterior cingulate gyrus: Evidence for an immune-modulated glutamatergic neurotransmission? J Neuroinflammation. 2011;8: 94.
5. Rommelfanger KS, Weinshender D. Norepinephrine: The redheaded stepchild of Parkinson's disease. Biochem Pharmacol. 2007;74(2):177–190.
6. Hosoi T, Nomura Y. Functional role of acetylcholine in the immune system. Front Biosci. 2004 Sep 1;9:2414–2419.
7. Rosas-Ballina M, Olofsson PS, Ochani M, et al. Acetylcholine-synthesizing T cells relay neural signals in a vagus nerve circuit. Science. 2011 Oct 7;334(6052):98–101. doi:10.1126/science.1209985. Epub 2011 Sep 15.

Dr. Chenggang Jin holds a PhD in immunology and is also an MD with 10 years of experience in medical research at Princeton University, the University of Iowa Hospitals and Clinics, and Beth Israel Deaconess Medical Center/Harvard Medical School. Dr. Jin also holds certification from the Educational Commission for Foreign Medical Graduates in the field of medicine. His specialized training includes many years of technical and research experience in cellular immunology and molecular biology. He also has extensive experience with flow cytometry and PCR instrumentation. He is currently the director of laboratory immunology at Pharmasan Labs and led the creation of a new clinical laboratory assay, iSpot-Lyme, for Lyme disease.
 Deanna Fall is currently a scientific writer and research analyst for NeuroScience Inc. and holds a bachelor's degree in biology from Ferris State University in Big Rapids, Michigan. Deanna joined NeuroScience in 2009 with experience in pharmaceutical research and development in the field of neurotoxicology. She is currently pursuing a master's degree in health informatics at the University of Minnesota. Deanna Fall is currently a scientific writer and research analyst for NeuroScience Inc. and holds a bachelor's degree in biology from Ferris State University in Big Rapids, Michigan. Deanna joined NeuroScience in 2009 with experience in pharmaceutical research and development in the field of neurotoxicology. She is currently pursuing a master's degree in health informatics at the University of Minnesota.
|
![]()
![]()






 Deanna Fall is currently a scientific writer and research analyst for NeuroScience Inc. and holds a bachelor's degree in biology from Ferris State University in Big Rapids, Michigan. Deanna joined NeuroScience in 2009 with experience in pharmaceutical research and development in the field of neurotoxicology. She is currently pursuing a master's degree in health informatics at the University of Minnesota.
Deanna Fall is currently a scientific writer and research analyst for NeuroScience Inc. and holds a bachelor's degree in biology from Ferris State University in Big Rapids, Michigan. Deanna joined NeuroScience in 2009 with experience in pharmaceutical research and development in the field of neurotoxicology. She is currently pursuing a master's degree in health informatics at the University of Minnesota.