|
Page 1, 2, 3
Your Patient Tells You That They Have Fibromyalgia; Now What?
So your patient says that they have fibromyalgia (FM) and were told that there is no known cause or cure. The best that their family physician can do is suggest that they take some prescription medications and learn to live with the pain. Should they, and you, accept this diagnosis and prognosis?
Before we answer that question, read a few real-life stories from these patients below:
- I was diagnosed with fibromyalgia and suffered with widespread pain, fatigue, and inability to lose weight. After two years of unsuccessfully trying different pain and antidepressant medications, I finally got a second opinion and was diagnosed with a previously undetected thyroid problem. My fibromyalgia pain went away completely after I was put on thyroid hormone replacement.
- I suffered with terrible fatigue and achiness throughout my body, but especially in my legs. My doctor told me that I had fibromyalgia and gave me an antidepressant. At the same time, one of my best friends told me that she had the same symptoms, but that her pain turned out to be related to her cholesterol medication. I asked my doctor about this and he took me off Lipitor, and within 2 months my fibromyalgia pain went away.
- I suffered with pain in multiple joints and my doctor checked for rheumatoid arthritis, which was negative. I was told that I had fibromyalgia and was put on pain medications. After a few months, I went to a rheumatologist who did new blood tests and found that I had inflammation somewhere in my body. More blood tests confirmed that I had Lyme disease. I was put on an antibiotics protocol and my fibromyalgia pain went away completely.
- I was diagnosed with fibromyalgia after my doctor ran numerous blood tests and could not find any medical problem that could explain my severe fatigue and widespread pain. I did notice that my symptoms got much worse around the time that my husband was diagnosed with prostate cancer. I was not sleeping through the night and started to develop panic attacks. My doctor recommended that I take a muscle relaxant before bedtime to improve my sleep and a low-dose antidepressant to help reduce my anxiety. In addition, I decided to take some yoga classes and cut back on the amount of coffee that I was drinking, both of which seemed to help reduce my stress levels. Now my fibromyalgia pain is greatly reduced and I am starting to feel normal again.
Each of these stories had a happy ending. Why? Because the doctor eventually figured out what was causing symptoms that were labeled, correctly or incorrectly, as fibromyalgia. Proper diagnosis is half the cure. If the diagnosis is not correct, how can the treatment be correct?
Proper Diagnosis
So, was the diagnosis of fibromyalgia correct in all these cases? If all of the patients suffered from the same condition, why did they require such different treatments? In the first three cases, the patient was incorrectly given a diagnosis of FM, and then another medical condition was eventually found that accounted for the symptoms of widespread pain and fatigue. The pain and fatigue went away in each of these cases, because proper diagnosis led the doctor to prescribe the proper treatment and medication.
FM is the correct diagnosis only when truly global pain and persistent fatigue are present, along with other centrally mediated problems such as anxiety, depression, irritable-bowel-like symptoms, and unrefreshed sleep, and other medical conditions that may explain the symptoms have been ruled out. As we can see in the first three cases above, the doctor gave the diagnosis of FM prematurely – before exploring all other possible causes for the pain and fatigue. Only in the last case was the patient correctly given a diagnosis of FM, after all other medical conditions were excluded and eliminated.
This last patient fits the classic profile of a FM patient as first described by the American College of Rheumatology in 1990, when the criteria for making a diagnosis of FM were first published.1 These diagnostic criteria were revised in 2010 and again modified in 2011.2 We have decided to use the term classic FM to describe this type of patient who has undergone extensive medical testing to rule out all possible medical diseases, as well as functional and metabolic issues, that could be causing the symptoms of widespread pain and fatigue. This is a very important and critical point: that the diagnosis of classic FM can only be made when there is no other disease(s) or disorder(s) present that could account for the symptoms.
In our previous examples, the patients clearly had other medical problems that were causing their symptoms of widespread pain and fatigue. The first patient had an underactive thyroid condition and was not suffering from classic FM. The second was experiencing a reaction to cholesterol-lowering medications and was not suffering from classic FM. The third patient had Lyme disease, and was not suffering from classic FM. Essentially those three patients were misdiagnosed with FM when in fact they had other medical problems that accounted for their symptoms.
So why do we have a dilemma? Doctors often use the single word fibromyalgia to diagnose a complex of symptoms that can have multiple causes. Worse yet, doctors often prescribe the same treatment package to all the patients whom they label with fibromyalgia. It is like using the term back pain and prescribing muscle relaxants to all patients with back pain. Some may have strained muscles, some may have arthritis, some may have herniated discs, and a few may even have a hidden fracture or dislocation. Sometimes the one-size-fits-all prescription may help patients get better, but not usually.
As a standard course in treating classic FM, most doctors will prescribe a combination of the following three treatments: (1) medications for sleep, pain, anxiety, and/or depression; (2) mild exercise for relaxing the muscles and to promote better blood flow; and (3) psychological counseling or relaxation techniques for reducing the emotional distress associated with fibromyalgia.3
In fact, these three treatments can be very helpful for a patient who is truly suffering from classic FM. We'll talk a lot more about classic FM in the next page or two, but for now it is important to know that only a small number of patients diagnosed with FM actually suffer from this classic variety of the syndrome. Most people who are told they have FM are really suffering from another problem. A study by Fitzcharles et al. revealed that patients diagnosed with FM by primary care physicians and rheumatologists ended up with an incorrect diagnosis a staggering 66% of the time when evaluated subsequently by a panel of FM experts.4 There are three broad categories of these conditions – other than classic FM – that are most often the cause of widespread pain and fatigue:5
1. Medical problems that may cause widespread pain and fatigue: examples are thyroid disease, diabetes, Lyme disease, cancer, and other medical diseases;
2. Musculoskeletal problems that may cause widespread pain and fatigue: examples are trigger points or "muscle knots," spinal joint problems such as disc degeneration and pinched nerves.
3. Functional/metabolic problems that may cause widespread pain and fatigue: examples are subtle functional hypothyroidism, in-efficiency of energy production in the cells of the body due to mitochondrial dysfunction, nutritional deficiencies (including vitamin D, CoQ10, carnitine, B vitamins, magnesium, etc.), chemical and food sensitivities, reactions to medications, and other problems with body metabolism and biochemistry.
Unfortunately, the standard treatment approach for classic FM will not help patients with pain and fatigue caused by conditions within any of these three categories.6 So what's the solution to this dilemma? Actually the answer is simple. The doctor needs to find the cause of the widespread pain and fatigue, and prescribe treatments that eliminate the cause. It doesn't help to have a doctor tell the patient they have fibromyalgia without first ruling out a condition in one of these other three categories of medical problems. However, if the doctor has performed an extensive medical history and laboratory tests, and still cannot find a cause for these symptoms, the patient may indeed be suffering from classic FM. We will now provide a brief explanation of classic FM.
Classic Fibromyalgia
The actual cause of classic FM is unknown, but is theorized to be an unusually strong response by the nervous system to physical and/or emotional trauma. Some people develop classic FM after a severe car accident, work-related injury, serious surgical procedures, physical or emotional abuse, or witnessing a horrific event. These traumatic events may lead to a heightened and prolonged pain response to many sorts of stimuli that would not normally be perceived as painful, such as bright lights, sounds, changes in temperature, moderate pressure on the skin or muscles, or household chemicals. Many researchers now believe that there is a strong genetic predisposition to the development of classic FM, because it tends to run in families, but clearly the right constellation of environmental factors also have to be present.8
In addition to living with chronic pain and fatigue, many classic FM patients have extraordinary amounts of stress in their lives or may have experienced intensely emotional events that have caused their nervous systems to have heightened responses to pain (similar to people who experience posttraumatic stress disorder [PTSD]). It is important to realize that these patients are not suffering from some sort of psychological defect; classic FM patients are not "imagining" their pain. The pain is quite real, and researchers can see abnormal changes in pain processing in the brains of classic FM patients with a special type of MRI scanning known as functional MRI (fMRI).9
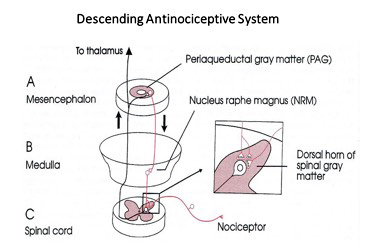
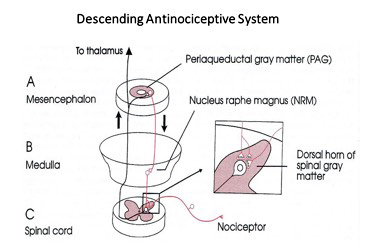
For some unknown reason, the brains of classic FM patients do not process pain in the same way as healthy patients without FM. Research has also shown that there is a lower amount of certain chemicals in the brain fluids of classic FM patients, which could explain the heightened pain responses and lead to failure of the descending antinociceptive system (DANS).7 (See Figure 1.) This is why certain prescription medications and nutraceuticals can help to reduce these chemical imbalances and thereby relieve the chronic pain of FM.3 Because the underlying cause of classic FM seems to be related to emotional stress or previous traumatic experiences, the most effective treatment is a combination approach that incorporates medication/supplementation, exercise, and relaxation techniques.10
Figure 1
Page 1, 2, 3
|
![]()
![]()
![]()