|
Fibromyalgia is a complex disorder characterized by fatigue, widespread pain, abnormal pain processing, sleep disturbance, and cognitive impairment.1 Diagnosis is made by exam and history, with 11/18 tender points positive, and is based on the new criteria developed in 2010 by the American College of Rheumatology (ACR). This consists of the Widespread Pain Index (score >7), a Symptom Severity Scale (score ≥5), the presence of symptoms for at least 3 months, and no comorbidity that would explain the pain.2
There is no lab test for fibromyalgia, leading some clinicians to doubt the existence of the condition. It presents a diagnostic and treatment challenge. Most fibromyalgia patients are women (female:male ratio 7:1), although men and children can have the disorder. Prevalence is about 2%, or 7 to 10 million people in the US. Most people are diagnosed during middle age.1
Certain risk factors for fibromyalgia have been identified, including stressful or traumatic events, PTSD, repetitive work injuries, illnesses such as viral infections, other diseases such as systemic lupus erythematosus (SLE) and rheumatoid arthritis, and genetic predisposition. Fibromyalgia often co-occurs, up to 25% to 65%, with another rheumatological condition such as rheumatoid arthritis, SLE, or ankylosing spondylitis.1 Our patients regularly report that there was one event in their lives that after which they were never the same, and all their fibromyalgia symptoms worsened from then on. Examples include a difficult childbirth, a surgery with poor outcome, repeated surgeries, a moving vehicle accident, repeated musculoskeletal injuries, and assault.
This has led to the theory that fibromyalgia is an abnormality of the stress response system. Continuous activation of the fight-or-flight, sympathetic nervous system response to threat, below the level of conscious awareness, leads to constant biochemical cascade of stress hormones. This maladaptive response may lead to many of the fibromyalgia symptoms.3
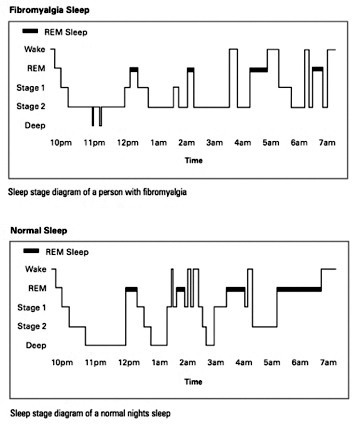
Sleep disturbances are another hallmark of the disorder. Patients report both trouble falling asleep and staying asleep, resulting in sleep deprivation no matter how many hours are spent in bed. They often say that they wake up in the morning feeling worse than when they went to bed. Others remark that they wake feeling as if they had been hit hit by a Mack truck or had run a marathon in their sleep.3
Human sleep is thought to be regulated by two systems, the circadian rhythm and sleep architecture. The circadian rhythm is the approximately 24-hour sleep/wake cycle. Sleep architecture is the brain wave organization of a sleep episode.4
Normal sleep architecture is characterized by predictable alteration between REM (rapid eye movement) and NREM (non-rapid eye movement) sleep during a sleep episode. NREM sleep occurs in four distinct brain wave patterns on an EEG. Stages 1 and 2 are the lightest levels of sleep and are associated with alpha and theta waves on the EEG. Stages 2 and 3 are deeper sleep, and associated with delta waves on the EEG. Sleep stages occur in cycles lasting 90 to 120 minutes each; four to five cycles occur during a normal night's sleep.4
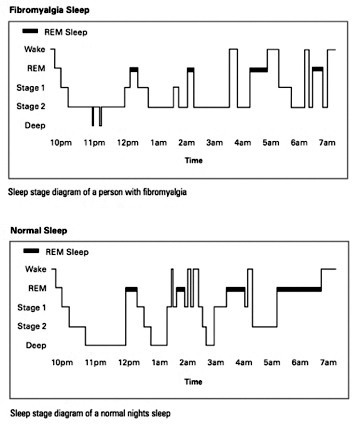
Sleep in fibromyalgia is disordered: the circadian rhythm is normal, but the sleep architecture is not.5,6 In fibromyalgia, there is evidence of prolonged sleep latency (time it takes to fall asleep), low sleep efficiency (total time spent asleep while in bed), and an increased amount of stage 1 NREM sleep.6 There is a reduction in slow wave sleep, as well as an increase in the number of arousals, and restless leg movement. Alpha wave activity is seen simultaneously with delta wave activity. This phenomenon is called phasic alpha, or alpha wave intrusion.6 It is associated with worsening of pain after sleeping. In one early study, a group of healthy volunteers underwent disrupted sleep similar to that seen in fibromyalgia patients. After three days, many of the volunteers exhibited fibromyalgia-like symptoms.7 Interestingly, phasic alpha sleep has also been reported in postinfectious and posttraumatic conditions, and chronic fatigue syndrome.6
There is compelling evidence that chronic, partial sleep deprivation results in a host of endocrine abnormalities. Evening cortisol is increased, leading to increased sympathovagal balance, with high sympathetic and lower parasympathetic tone. There is increased sleep latency. The normal nocturnal thyroid-stimulating hormone (TSH) level is decreased. The nocturnal release of growth hormone (GH) is decreased.8 (Growth hormone in adults is responsible for regulating the repair and maintenance of muscle.3) Leptin, a hormone released by fat cells to signal satiety to the brain, is decreased. Ghrelin, a peptide secreted by the stomach that stimulates appetite, is increased. Poor quality sleep is also associated with increased pain, decreased immune response, and IBS symptoms.8 We see many patients with abnormalities in all these areas.
In our clinic, sleep is usually the first thing that we work on, because improvement in sleep architecture can lead to profound symptom improvement. We screen for sleep apnea and restless legs syndrome, and get a sleep study if the screen is positive. Treating those conditions can also contribute greatly to symptom improvement.
The goal in treating the sleep disorder in fibromyalgia is to get the patient into deep, delta wave sleep. There is no one medicine that will put someone into that stage of sleep. One promising drug, Xyrem (sodium oxybate), was successful in trials in getting people into deep, delta wave sleep, but it was not approved by the FDA for use in fibromyalgia.9,10 In our clinic we combine conventional medicines to achieve easy sleep onset with a sedative, an anticonvulsant (to induce GABA activity), and a sympathetic nervous system dampener.
The pain in fibromyalgia is chronic pain.11 Chronic pain is pain that continues or recurs over a prolonged period and may or may not be associated with trauma or injury.12 There is evidence that innocuous inputs contribute to amplification of pain from the central nervous system.13 The central nervous system becomes exquisitely sensitive and tuned in to pain signals. Long-term treatment of chronic pain with opioids is contraindicated and can lead to opioid-induced hyperalgesia, which compounds the problem.14 Pain management is challenging. The buprenorphine patch (Butrans) is a promising new patch that is only a partial opioid agonist and seems to both be effective in fibromyalgia and have less association with opioid-induced hyperalgesia.15 Topical pain treatment creams, such as Voltaren gel and Pennsaid, are sometimes effective as well.
Fibromyalgia is considered a chronic condition with no real "cure." Many patients express frustration over their symptoms and continue to seek the one magic pill or treatment that will make all their symptoms disappear. Others try to reason their way out of their symptoms.
But the best long-term management of fibromyalgia symptoms is the development of robust life habits. We support the patient with modern medicines but actively recommend activities such as stress management, self-care, thoughtful exercise, yoga, and mindfulness practices. These are all evidence-based methods of turning down or even reversing the neuroplastic changes that occur in chronic pain patients and are completely appropriate for fibromyalgia patients as well.16,17 Several recent studies have identified yoga as an especially efficacious modality to use to alleviate fibromyalgia symptoms.18,19 In our clinic, we combine evidence-based medical treatment together with an on-site exercise studio where we offer classes in yoga and gentle movement, and support groups to facilitate the development of new, healthful habits.
As with diabetes or many other chronic conditions, there is no cure for fibromyalgia. There is, however, great potential for increased functionality and improvement in quality of life.

Notes
1. CDC. Fibromyalgia [online article]. http://www.cdc.gov/arthritis/basics/fibromyalgia.htm. Accessed June 23, 2012.
2. Wolfe F, Clauw DJ, Fitzcharles M-A, et al. Fibromyalgia criteria and severity scales for clinical and epidemiological studies. J Rheumatol. June 2011;38(6):1113-1122.
3. Liptan GL. Figuring Out Fibromyalgia: Current Science and the Most Effective Treatments. Visceral Books; 2011.
4. Pressman MR. Stages and architecture of normal sleep [online article]. UpToDate. 2012. http://www.uptodate.com/contents/stages-and-architecture-of-normal-sleep.
5. Klerman E, Goldenberg D, Brown E, Maliszewski A, Adler G. Circadian rhythms of women with fibromyalgia. J Clin Endocrinol Metab. Mar 1, 2001;86(3):1034-1039 .
6. Roizenblatt S, Moldofsky H, Benedito-Silva AA, Tufik S. Alpha sleep characteristics in fibromyalgia. Arthritis Rheum. 2001;44:222-230.
7. Moldofsky H, Scarisbrick P. Induction of neurasthenic musculoskeletal pain syndrome by selective sleep stage deprivation. Psychosom Med. 1976;38(1):35.
8. Goldberger J. Sympathovagal balance: how should we measure it? Am J Physiol. April 1, 1999;276(4):H1273-H1280.
9. Spaeth M, Bennett R, Benson A, Wang YG, Lai C, Choy E. Sodium oxybate therapy provides multidimensional improvement in fibromyalgia: results of an international phase 3 trial Ann Rheum Dis. doi:10.1136/annrheumdis-2011-20041.
10.FDA panel rejects Xyrem as fibromyalgia treatment [online article]. WebMD. http://www.webmd.com/fibromyalgia/news/20100820/fda-panel-rejects-xyrem-as-fibromyalgia-treatment. Accessed July 9, 2012.
11.Bennett R., Emerging concepts in neurobiology of chronic pain: evidence of abnormal processing in fibromyalgia. Mayo Clin Proc. 1999.
12.Chronic pain management [online article]. WebMD. http://www.webmd.com/pain-management/guide/understanding-pain-management-chronic-pain. Accessed July 5, 2012.
13.Woolf C, Doubell T. The pathophysiology of chronic pain - increased sensitivity to low-threshold AB-fibre inputs. Curr Opin Neurobiol. Aug 1994;4(4):525-534.
14.Angst M, Clark J. Opioid induced hyperalgesia: A qualitative systemic review. Anesthesiology. March 2006; 3:570-587.
15.Buprenorphine transdermal system [Web page]. www.butrans.com. Accessed July 10, 2012.
16.Holzel B, Carmody J, Evans K, et al. Stress reduction correlates with structural changes in the amygdala. Soc Cogn Affect Neurosci. 2010;5(1):11-17.
17.Vestergaard-Poulsen P, van Beek M, Skewes J, et al. Long-term meditation is associated with increased gray matter density in the brain stem. Neuroreport. Jan 2009;20(2):170-174.
18.Carson J, Carson K, Jones K, Bennet R, Wright C, Mist S. A pilot randomized controlled trial of the Yoga of Awareness program in the management of fibromyalgia. Pain. November 2010;151(2):530-539.
19.Hennard J.A protocol and pilot study for managing fibromyalgia with yoga and meditation.Int J Yoga Ther. 2011;(21):109-121.
 Val Cashman, PA-C, is a graduate of Pacific University's PA school. After forays into neurosurgery and hospital medicine, she has found her professional home at the Frida Center for Fibromyalgia in Portland, Oregon, where she joins a team of clinicians dedicated to the treatment and management of this complex chronic condition. When not at work, Val enjoys spending time with her family in their inner southeast Portland neighborhood. Val Cashman, PA-C, is a graduate of Pacific University's PA school. After forays into neurosurgery and hospital medicine, she has found her professional home at the Frida Center for Fibromyalgia in Portland, Oregon, where she joins a team of clinicians dedicated to the treatment and management of this complex chronic condition. When not at work, Val enjoys spending time with her family in their inner southeast Portland neighborhood.
|



![]()
![]()
![]()

 Val Cashman, PA-C, is a graduate of Pacific University's PA school. After forays into neurosurgery and hospital medicine, she has found her professional home at the Frida Center for Fibromyalgia in Portland, Oregon, where she joins a team of clinicians dedicated to the treatment and management of this complex chronic condition. When not at work, Val enjoys spending time with her family in their inner southeast Portland neighborhood.
Val Cashman, PA-C, is a graduate of Pacific University's PA school. After forays into neurosurgery and hospital medicine, she has found her professional home at the Frida Center for Fibromyalgia in Portland, Oregon, where she joins a team of clinicians dedicated to the treatment and management of this complex chronic condition. When not at work, Val enjoys spending time with her family in their inner southeast Portland neighborhood. 