by Keivan Jinnah, ND, MSOM, LAc
A new patient comes in to see you with recent lab results (CBC and CMP) in hand. Everything is within reference range except for a mild elevation of the ALT and AST (59 and 43 IU/l respectively). Her previous doctor told her not to worry about it, but she wasn’t comfortable with that advice. She is coming to see you to figure out why her liver enzymes are high. She feels fine but is worried by her high enzymes. What is the thought process you go through to evaluate what is going on?
This hypothetical (but very common) situation may present in many ways. My goal in this article is to walk through the thought process, differential, and lab testing involved in thoroughly evaluating an asymptomatic patient with abnormal liver chemistries.
First, a little bit about laboratory reference ranges or “normal” values. Reference ranges are not based on optimal ranges, or even necessarily healthy ranges. Each laboratory establishes its ranges based on a bell curve of all the people tested in that lab company. The reference range is set at 2 standard deviations from the mean, which, by definition, includes 95% of all people tested. This is why some labs will have upper normal limits of AST and ALT in the 40s IU/l, while others will be up to the 50s or 60s IU/l. I can’t help but think about all of the occult chronic hepatitis C infection, endemic fatty liver disease, and polypharmacy usage in the population driving up the mean level of liver enzymes. We know how important healthy liver function is for maintaining homeodynamic balance and health in the body. I want my patients’ liver enzymes to be optimal, not just within a range of mostly ill people, and if the enzymes are higher than that, I want to know why.
What are optimal liver enzyme levels? Fortunately, there have been a few good studies looking at this question and how the optimal ranges differ for women and men. One large study published in 2004 looked at 94,533 men and 47,522 women in Korea aged 35-59 years old.1 They looked at the connection between a normal range of serum aminotransferase concentration and mortality from liver disease according to death certificate. What they found is that there was a positive association between the aminotransferase concentration, even within normal range (35-40 IU/l), and increased mortality from liver disease. Compared with <20 IU/l,the relative risks of dying from liver disease for an AST concentration of 20-29 IU/l and 30-39 IU/l were 2.5 and 8.0 in men and 3.3 and 18.2 in women, respectively. The corresponding risks for ALT were 2.9 and 9.5 in men and 3.8 and 6.6 in women, respectively. The study concluded that the best cut-off values for the prediction of liver disease in men were 31 IU/l for ASTand 30 IU/l for ALT. The study was not able to calculate best cut-off values for women due to insufficient data; but it is clear, and concluded by the researchers, that the optimal values for women would be lower than for men, especially for AST.
In 2017 the American College of Gastroenterology (ACG) published its assessment for optimal liver chemistry ranges.2 The ACG stated that multiple studies have demonstrated that an elevated ALT has been associated with increased liver-related mortality and that a true healthy normal ALT level ranges from 29 to 33 IU/l for males, 19 to 25 IU/l for females. The ACG recommended evaluation of any patient with liver chemistries above those optimal values.
Both ALT (formerly SGPT) and AST (formerly SGOT) exist in highest quantity in the hepatocytes of the liver. ALT is found almost exclusively in the hepatocytes whereas AST is also found in significant quantities in other cells of the body. AST outside of the liver, in descending order of quantity, is found in cardiac muscle, skeletal muscle, kidneys, brain, pancreas, lungs, leukocytes, and erythrocytes. For this reason, an elevated AST may be the result of breakdown of one of these extra-hepatic tissues whereas ALT is much more specific to damage in the liver.
An isolated elevation of AST is worrisome for muscle breakdown (consider injury, extreme exercise, polymyositis), or cardiac muscle deterioration (high isolated AST has been used historically as a marker for possible myocardial infarction), acute hemolytic anemia, acute pancreatitis, and acute renal disease. The healthy upper limit of AST for males is higher than that for females because, as a population average, males have higher muscle mass which will contribute to higher normal AST levels. This would be true of any larger person, regardless of gender. Said in a different way, a high normal or mildly elevated AST in a woman, or smaller person, is more clinically significant and in need of investigation.
The most common cause of asymptomatic
high enzymes is fatty liver disease.
If both AST and ALT are elevated, then liver inflammation is almost certainly the source. Alkaline phosphatase (ALP), gamma-glutamyl transferase (GGT), and bilirubin should be looked at for concomitant elevations as markers of inflammation and stasis in the biliary tree system. Elevations of GGT in addition to elevated ALP will help identify the ALP as coming from the liver as opposed to bone. A higher ALP elevation in relation to liver enzyme elevation will indicate primarily a biliary tree inflammation, and conditions involving cholestasis should be investigated, including primary biliary cholangitis (PBC – previously called primary biliary cirrhosis), primary sclerosing cholangitis (PSC), cholelithiasis, stricture, and cancer. Higher liver enzyme elevation relative to ALP will indicate a primarily hepatocyte injury. In hepatocyte injury, ALT will typically be elevated higher than AST (because of greater ALT in the liver cells), but important exceptions are alcoholic hepatitis, Wilson’s disease, and potentially liver cirrhosis and liver cancer. Alcoholic liver disease has a classic reversed ratio of AST>ALT, often ≥ 2:1. This is due to alcohol’s depletion of pyridoxal-5-phosphate that is a necessary cofactor in the production of ALT.
The classic differential for mild transaminase elevation, defined as <5x above normal limit, (which we know now is really any liver enzyme between 30-150 IU/l) is
· Fatty liver,
· Alcoholic liver disease,
· Chronic viral hepatitis B or C ,
· Pharmaceutical, OTC, street drug, or herbal supplement reaction,
· Hemochromatosis (autosomal recessive, homozygous 1/400, heterozygous 1/12),3
· Neoplasm,
· Autoimmune liver disease,
· Biliary cholangitis,
· Wilson’s disease, and
· Alpha-1 antitrypsin deficiency.
Other causes of mildly elevated liver enzymes that are often overlooked in the classical differential include the following:
· Acute or chronic infection with EBV and other herpes strain viruses such as cytomegalovirus,
· Environmental or heavy metal hepatotoxicity,
· A highly processed or fast food diet,
· Gluten sensitivity,
· Thyroid disease (hypo or hyper), and
· Tick-borne disease.
Any and all these things may result in increased hepatocyte membrane injury, leading to an increase of transaminase enzymes being dumped into the blood stream. The short way of saying this is that they all create liver inflammation. The reality, of course, is that many patients have more than one thing inflaming their liver. A good history and some follow-up lab work should help focus in on the singular, or multiple, causes of the liver inflammation and help determine whether a liver biopsy is necessary for definitive diagnosis or evaluation of the extent of the liver damage.
In terms of prevalence, (in order to keep our eyes on the horses before we go chasing the zebras), the most common cause of asymptomatic high enzymes is fatty liver disease (FLD), followed by chronic viral hepatitis (CVH), then alcohol-related liver disease (ALD). A 1996 review of four studies found asymptomatic elevation of liver enzymes was due in 42% of cases to FLD, in 24% of cases to CVH, in 14% to ALD, in 11% to rare liver disease or no cause found, and in 7% to liver cirrhosis.4 The rare liver diseases included drug reactions, hemochromatosis, alpha-1 antitrypsin disease, biliary cirrhosis, Wilson’s disease, sclerosing cholangitis, granulomatous colitis, sarcoidosis, and extrahepatic obstruction. Other studies have found that the prevalence of the cause of elevations of enzymes depends greatly on the population studied.5 With those top three conditions responsible for roughly 80% of cases, they need to be ruled out first. One of the difficulties posed is that the definitive diagnosis of FLD requires a liver biopsy, and it is debatable if that intervention is warranted. There are many less invasive clues that will indicate the likelihood of fatty liver disease and may inform the need for that intervention. Thorough work up and exclusion of other conditions is still necessary to clarify all contributing causes and to prioritize action.
Back to our hypothetical patient: Is an ALT of 59 and an AST of 43 IU/l something to investigate? Absolutely.
The steps of how I would evaluate any patient presenting with a mild (30-150 IU/L) to moderate (150-450 IU/L) elevation of their ALT and AST would look like the following (See Figure 1):
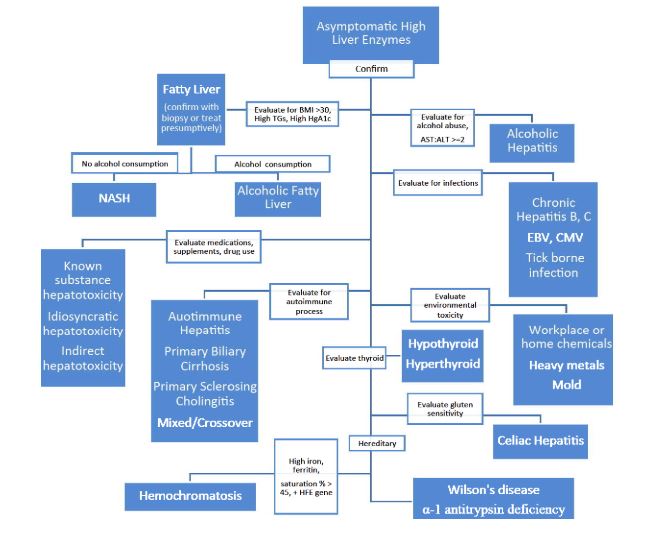
1. Confirm high liver enzymes with follow up test. Not necessary if patient has had repeated history of high enzymes.
2. To save on time and blood draws, include the second level of tests at this time, including lipid panel (looking for elevated fasting triglycerides), HgA1c, fasting glucose and fasting insulin (helpful in evaluating the likelihood of FLD); hepatitis C Ab, hepatitis B sAg, sAb, cAb (CVH); tTg IgA and IgG, DGP IgA and IgG, total SIgA (celiac disease/gluten sensitivity); serum iron, TIBC, transferrin saturation %, and ferritin levels (hemochromatosis); ANA and F-actin antibody (autoimmune hepatitis), serum ceruloplasmin (Wilson’s disease), and full thyroid panel. Consider serum protein electrophoresis (marked decrease in alpha-globulin bands suggests alpha1-antitrypsin deficiency).
Depending on history, I may also consider hormone evaluation, especially looking for low testosterone in middle-aged men as a risk factor for FLD.6
3. Evaluate patient’s diet, BMI, and blood sugar control as risk factors for FLD as well as inflammation due to nutrient-poor, highly processed food diet. Indications of FLD include elevated fasting triglycerides, high HgA1c,7 higher waist circumference, elevated fasting insulin, and elevated body mass index.8 We know that FLD is strongly associated with insulin resistance, diabetes, and obesity.9,10 Consumption of alcohol may contribute to the development of FLD, but it is not a necessary component. Non-alcoholic steatohepatitis (NASH) is strongly linked to obesity, blood sugar dysregulation and insulin resistance, independent of alcohol.11 Further workup to establish the presence of insulin resistance and diabetes should be done.
4. If the AST:ALT ratio is ≥2:1, then strongly consider the likelihood of ALD. Greater than 90% of patients with >2:1 ratio of AST:ALT were found to have ALD.12 This potential cause of high enzymes will need to be evaluated with a good history and discussion with the patient. Alcohol consumption is notoriously underreported by patients. (One rule of thumb is to take what a patient tells you and multiply by 5.) One lab marker that may indicate chronic alcohol abuse is an elevated GGT. This enzyme is very sensitive to alcohol but is not specific. GGT is also raised in pancreatic disease, myocardial infarction, renal failure, COPD, diabetes, and certain medications, including phenytoin and barbiturates.13 If the patient is a heavy alcohol user, or alcoholic, then that would be the primary issue to address to reduce liver inflammation even if other things are going on. Naltrexone may be helpful to reduce the patient’s alcohol cravings.
5. If testing is positive for either chronic hepatitis B or C, then evaluation for conventional antiviral therapy is warranted. A positive HBVsAg indicates current hepatitis B infection. A positive HBVsAb indicates past cleared infection or past immunization to hepatitis B. A positive HBVcAb indicates a past infection.
6. Medications, supplements, and street drugs need to be evaluated for contributing to, or causing, liver inflammation in our patients. The National Institutes of Health website LiverTox (http://livertox.nih.gov) lists over 1200 agents, including prescription and over-the-counter medications, herbal products, nutritional supplements, metals, and toxins, and describes their potential to cause liver injury; 447 prescription drugs have been implicated in at least one published case of liver injury.14 There are three types of drug or herbal induced liver injury: direct, idiosyncratic, and indirect.15
Direct hepatotoxicity is caused by medications and other substances that have an intrinsically toxic effect to the liver. This toxicity is dose dependent, predictable, and reproducible in animal models.15 The drugs most associated with this direct hepatotoxicity are high doses of acetaminophen, aspirin, niacin, amiodarone, and many antineoplastic agents, as well as intravenous buprenorphine, methylprednisolone and tetracycline.14
Special attention needs to be paid to acetaminophen-containing products as they are available over-the-counter in many forms and are responsible for more than 56,000 emergency room visits, 2,600 hospitalizations, and an estimated 458 deaths due to acute liver failure each year in the US as of information published in 2004.16 The US Acute Liver Failure Study Group registry of more than 700 patients with acute liver failure across the United States implicates acetaminophen poisoning in nearly 50% of all acute liver failure in this country.16The hepatotoxic potential of acetaminophen is magnified greatly if it is used in conjunction with alcohol, or by someone who is a chronic user of alcohol, due to the depletion of glutathione that is needed for acetaminophen detoxification. As William Lee asked in his article in Hepatology in 2004 in regards to the incredible human toll and hepatotoxicity of acetaminophen: “Is this amount of injury and death really acceptable for an over-the-counter pain reliever?”16
The number of cases of liver toxicity as a result of herbal or supplement ingestion is very small in comparison to that of acetaminophen, but they seem to receive an outsized amount of attention and reaction. Table 1 shows the botanical medicines most associated with hepatotoxicity.
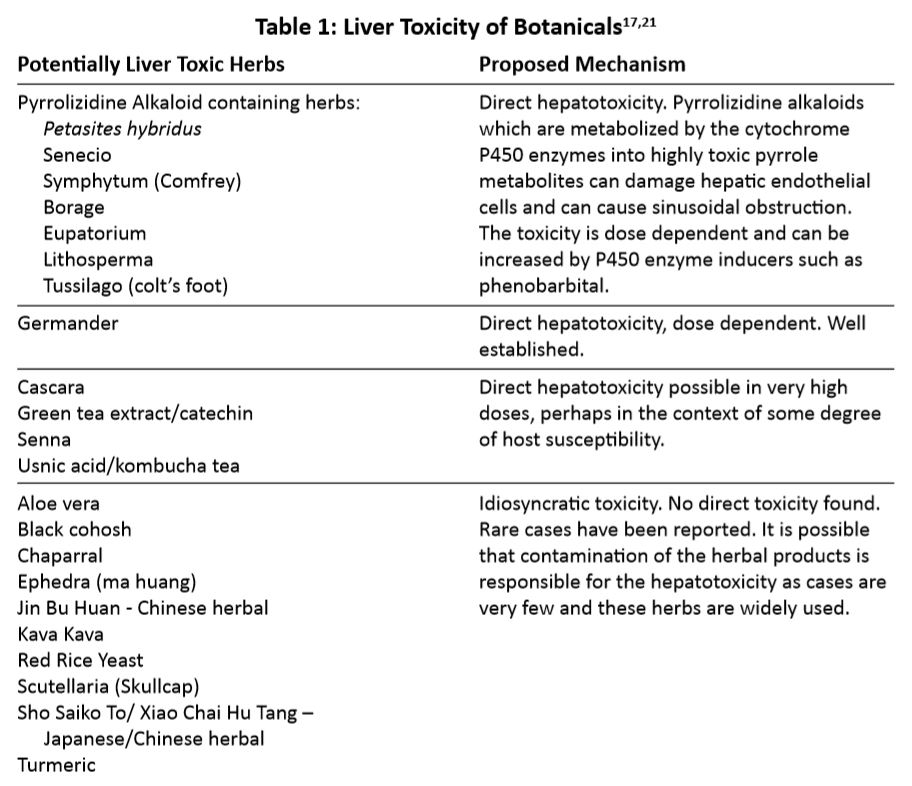
Idiosyncratic hepatotoxicity involves substances that have little or no intrinsic liver toxicity but can cause liver toxicity in rare cases. (1 in 2000 to 1 in 100,000 patient exposures).15 These injuries are not dose-dependent, not predictable and not reproducible in animal models. The prescription drugs that are most likely to cause idiosyncratic hepatotoxicity, in descending order of reported cases, are amoxicillin-clavulanate, isoniazid, nitrofurantoin, TMP-SMZ, minocycline, cefazolin, azithromycin, ciprofloxacin, levofloxacin, diclofenac, phenytoin, methyldopa, and azathioprine.15 It is important to note that nine of the top ten drugs reported are antimicrobial agents, mostly antibiotics. The cholesterol lowering statin class of medications appears to have both mild direct as well as idiosyncratic liver toxicity.17
The third, and more recently recognized, category is indirect drug-induced liver injury.15 These medications result in an induction or exacerbation of a liver disease rather than injuring the liver directly. Examples include risperidone, lomitapide, and glucocorticoids worsening fatty liver disease because of their effect on weight gain, or triglycerides, or insulin sensitivity. Another example is anticancer chemotherapeutic agents or corticosteroids reactivating a hepatitis B infection resulting in acute hepatitis. A third example is immunomodulating agents, such as monoclonal antibodies or interferon, creating immune-mediated liver injury.15
In a patient with unexplained liver enzyme elevations, I recommend discontinuing any medications, supplements, and drugs, that are not absolutely necessary with extra attention to those more recently added to the patient’s regimen.
The next steps of how I would evaluate any patient presenting with a mild (30-150 IU/L) to moderate (150-450 IU/L) elevation of their ALT and AST include the following:
7. Exposure to environmental toxicity, including workplace and home chemicals, heavy metals, and mold should also be assessed. History is very important here. The different lab assessments available for such toxicity is a topic much discussed in the Townsend Letter, and I will not enter the discussion here other than to bring attention to the hepato-inflammatory potential of these toxins.
8. Don’t forget the possibility of dietary gluten as a cause of your patient’s liver inflammation. Celiac disease was found to be present in about 9% of patients with chronic unexplained liver enzyme elevation.18 In another study, it was found that isolated transaminitis with nonspecific histological changes in a liver biopsy is the most common hepatic presentation of celiac disease.19 Gluten reactivity also frequently co-exists with autoimmune liver disease.19 In the studies that I reviewed that looked at different causes of asymptomatic liver enzyme elevations, there is always a percentage that are found to be of unknown cause, typically in the high single digits. Rarely in these studies is gluten sensitivity or celiac disease tested as a potential cause. I think it is very possible that gluten sensitivity, and the resultant hepatic inflammation, may account for at least part, if not all, of the “unknown cause” found in these studies.
I believe that gluten sensitivity exists on a continuum, with celiac disease in its most extreme form on one end and mild non-celiac gluten sensitivity (NCGS) on the other end. There are many shades of intensities as we move from one end of the spectrum to the other. It makes complete sense to me that the hepatic inflammatory potential of gluten can exist anywhere on this continuum and is not reserved for only the most extreme gluten sensitivity (ie. celiac disease). Based on this, laboratory testing for gluten sensitivity, in the context of liver inflammation, is challenging. Standard screening tests for celiac disease include tissue Transglutaminase (tTG) and deaminated gliadin peptide (DGP) antibodies in the serum. These antibodies should be tested with the patient eating gluten in their diet for at least four weeks prior to testing. A definitive diagnosis of full-blown celiac requires a small intestinal biopsy with visualized villous atrophy. My concern here is that many people are not at the far end of the spectrum and that these tests will not capture the patient who has NCGS and reactive enough to gluten that its consumption is resulting in liver inflammation.
We know that eating a gluten-free diet normalizes liver enzymes and histological changes in celiac patients.19 I will often recommend that patients adopt a gluten-free, whole foods diet while we are determining the cause of their high enzymes.
9. After two-to-three months of gluten-free whole foods diet and elimination of potentially hepato-inflammatory medications and supplements, retest patient’s liver enzymes.
10. If the patient has been compliant and enzymes are still elevated and the first level of lab testing did not uncover an explanation, then consider the next level of testing. This would include Epstein Barr virus comprehensive panel, including early antigen as an indication of reactivation of the virus, Cytomegalovirus, and possibly other herpes strains. Mild liver disease can be produced by all the human herpesviruses in the course of systemic illness.20
11. If other causes have been excluded and/or history warrants, then tick-borne infections should also be considered as a cause of liver inflammation. Again, testing is imperfect and, in these infections, expensive. I would want a stronger clinical case than just mildly elevated liver enzymes to justify pursuing this path.
Through the process of differentiating, we may employ imaging or liver biopsy. A liver ultrasound is minimally invasive and will help with the diagnosis of fatty liver disease as well as liver tumor and cholelithiasis. A liver biopsy is sometimes needed for definitive diagnosis (fatty liver disease, cancer, alcoholic liver disease) and is often employed both to confirm diagnosis and to assess the degree of fibrosis and inflammation in the liver from the disease process. Utilization of these procedures will depend on the uncertainty of the diagnosis and the chronicity of the liver enzyme elevation.
As wholistic practitioners we know how vital the liver is (the only organ with the word “live” in it) in keeping us healthy. Any elevation of liver enzymes in your patient should be investigated.
References
1. Chang Kim Hyeon, et al. Normal serum aminotransferase concentration and risk of mortality from liver diseases: prospective cohort study. BMJ. 2004;328:983.
2. Kwo P, et al. ACG clinical guideline: Evaluation of abnormal liver chemistries. Am J Gastroenterol. 2017;112:18–35.
3. Steinberg KK, et al. Prevalence of C282Y and H63D mutations in the hemochromatosis (HFE) gene in the United States. JAMA. 2001;285:2216-22.
4. Theal RM, Scott K. Evalutating asymptomatic patients with abnormal liver function test results. Am Fam Phys. 1996; 53: 2111-9. (cited in Yarnell, E, Naturopathic Gastroenterology; Naturopathic Medical Press, c.2000: pg. 319).
5. Katkov WN, et al. Elevated serum alanine aminotransferase levels in blood donors: the contribution of hepatitis C virus. Ann Intern Med. 1991;115:882-4.
6. Mody A, et al. Relevance of low testosterone to non-alcoholic fatty liver disease. Cardiovasc Endocrinol. 2015;4:83–9.
7. Han Ma, et al. Independent association of HbA1c and nonalcoholic fatty liver disease in an elderly Chinese population. BMC Gastroenterol. 2013;13:3.
8. Loomis AK, et al. Body mass index and risk of nonalcoholic fatty liver disease: Two electronic health record prospective studies. J Clin Endocrinol Metab. March 2016; 101: 945–952.
9. Rhee EJ. Nonalcoholic fatty liver disease and diabetes: An epidemiological perspective. Endocrinol Metab (Seoul). 2019;34:226-33.
10. Lonardo A, et al. Fatty liver is associated with an increased risk of diabetes and cardiovascular disease – Evidence from three different disease models: NAFLD, HCV and HIV. World J Gastroenterol. 2016;22:9674–93.
11. Firneisz, G. Non-alcoholic fatty liver disease and type 2 diabetes mellitus: The liver disease of our age? World J Gastroenterol. 2014; 20:9072–89.
12. Cohen JA, Kaplan MM. The SGOT/SGPT ratio – an indicator of alcoholic liver disease. Dig Dis Sci. 1979;24:835-8.
13. Pratt DS, Kaplan MM. Evaluation of abnormal liver-enzyme results in asymptomatic patients. NEJM. 2000;342:1266-71.
14. Bjornsson ES, Hoofnagle JH. Categorization of drugs implicated in causing liver injury: critical assessment based on published case reports. Hepatology. 2016: 63:590-603.
15. Hoofnagle JH, Bjornsson ES. Drug-Induced Liver Injury – Types and Phenotypes. N Engl J Med. 2019;381:264-73.
16. Lee WM. Acetaminophen and the U.S. acute liver failure study group: lowering the risks of hepatic failure. Hepatology. 2004;40:6 –9.
17. National Institutes of Health. LiverTox: Clinical and research information on drug-induced liver injury [Internet]. [Online] April 10, 2018. [Cited: October 19, 2019.] https://www.ncbi.nlm.nih.gov/books/NBK548441/.
18. Bardella MT, et al. Chronic unexplained hypertransaminasemia may be caused by occult celiac disease. Hepatology. 1999; 29: 654–7.
19. Rubio-Tapia A, Murry JA. The liver in celiac disease. Hepatology. 2007; 46: 1650-8.
20. Fingeroth JD. Herpesvirus infection of the liver. Infec Dis Clin Nort Amer. September 2000;14:689-719.
21. Schiano TD. Hepatotoxicity and complementary and alternative medicines. Clin Liver Di. 2003;7: 453-73.
Keivan Jinnah, ND, MSOM, LAc, is a naturopathic physician, licensed acupuncturist, and a board-certified Chinese herbalist. He completed a four-year doctorate of naturopathic medicine and a three-year masters of science in Oriental medicine at the Natural College of Naturopathic Medicine (NCNM) in Portland, Oregon. His thesis work investigated both naturopathic and Chinese medicine treatments for hepatitis C and chronic liver disease.
Dr. Jinnah has lectured to the hepatitis C community and taught hepatology at the NCNM. His research on this condition is scheduled to be published in the peer-reviewed Journal of Naturopathic Medicine.
Dr. Jinnah is in private practice at Clinton Street Health Care in Portland, Oregon, where he continues to lecture and synthesize Eastern and Western natural treatments for hepatitis C