Reprinted online
only from Environmental
Health Perspectives. March 1997; Vol. 105, Supplement 2
and Townsend Letter for Doctors and Patients.
210:76-84 (January 2001).
Page 1, 2 
Abstract: This
paper attempts to clarify the nature of chemical sensitivity by proposing
a theory of disease
that unites the disparate clinical
observations associated with the condition. Sensitivity to chemicals
appears to be the consequence of a two-step process: loss of tolerance
in susceptible persons following exposure to various toxicants, and
subsequent triggering of symptoms by extremely small quantities of
previously tolerated chemicals, drugs, foods, and food and drug combinations,
including caffeine and alcohol. Although chemical sensitivity may be
the consequence of this process, a term that may more clearly describe
the observed process is toxicant-induced loss of tolerance. Features
of this yet-to-be-proven mechanism or theory of disease that affect
the design of human exposure studies include the stimulatory and withdrawal-like
nature (resembling addiction) of symptoms reported by patients and
masking. Masking, which may blunt or eliminate responses to chemical
challenges, appears to have several components: apposition, which is
the overlapping of the effects of closely timed exposures, acclimatization
or habituation, and addiction. A number of human challenge studies
in this area have concluded that there is no physiological basis for
chemical sensitivity. However, these studies have failed to address
the role of masking. To ensure reliable and reproducible responses
to challenges, future studies in which subjects are evaluated in an
environmental medical unit, a hospital-based facility in which background
chemical exposures are reduced to the lowest levels practicable, may
be necessary. A set of postulates is offered to determine whether there
is a causal relationship between low-level chemical exposures and symptoms
using an environmental medical unit. – Environ Health
Perspect 105(Suppl 2):445–453 (1997) 
Key
words: adaptation, chemical sensitivity, masking, multiple chemical
sensitivity, sensitivity, sensitization, tolerance, addiction, habituation

Introduction
Clinical observations in North America1-7 and Europe8 point
to an expanding group of patients who report sensitivities to extraordinarily
low levels
of environmental chemicals. This phenomenon, termed chemical sensitivity
or multiple chemical sensitivity, appears to develop de novo in some individuals
following acute or chronic exposure to a wide variety of environmental agents
including various pesticides, solvents, drugs, and air contaminants in so-called
sick buildings. Some practitioners have attributed a broad spectrum of chronic
medical conditions involving any and every organ system to chemical sensitivity
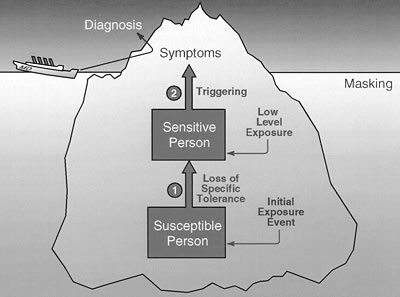
(Figure 1. Some conditions that
have been attributed to chemical sensitivity, 88KB .pdf).4
Efforts to formulate a case definition for chemical sensitivity, identify relevant
biomarkers, and explore a variety of mechanisms for the condition have escalated
over the past decade. Several conflicting schools of thought have evolved with
respect to underlying mechanisms, ranging from the purely psychological to
the wholly physiological. In the midst of the tumult surrounding chemical sensitivity
lies a profound but little-recognized scientific debate concerning the origins
of disease. Some participants in this debate are challenging currently accepted
notions concerning the causes for many chronic illnesses.
This paper attempts to clarify the nature of chemical sensitivity by describing
a general mechanism that appears to underlie these cases; proposes a theory
of disease based upon this general mechanism; and offers a set of testable
postulates for corroborating or refuting this theory. Science is not about
opinion or belief; it is about "guess and test," that is, formulating
hypotheses and then devising experiments to test them.

Terminology
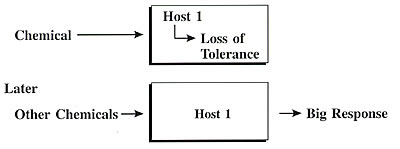
Phenomenologically, chemical sensitivity appears to develop in two stages.3,4
First is the loss of tolerance (possibly but not necessarily due to sensitization)
following acute or chronic exposure to various environmental agents such
as pesticides, solvents, or contaminated air in a sick building. Second is
the subsequent triggering of symptoms by extremely small quantities of previously
tolerated chemicals, drugs, foods, and food and drug combinations (Figure
2). Although sensitivity to chemicals may be one of the consequences of this
two-stage process, the term chemical sensitivity does not appropriately describe
the process involved.
There are two principal reasons for this.
First, although chemical sensitivity certainly sounds like an inconvenient
problem to have,
the words fail to convey
the potentially disabling nature of the condition and its postulated
origins in a toxic exposure. Some researchers balk at using the word
toxic in this
manner. However, numerous investigators from different geographic regions
have published strikingly similar descriptions of individuals
who report disabling
illnesses after exposure to recognized environmental contaminants, albeit
at levels not generally regarded as toxic.1,9-12 Yet, for these
individuals,
the
exposure appears to have been toxic. Figure 2: Phenomenology
of chemical sensitivity
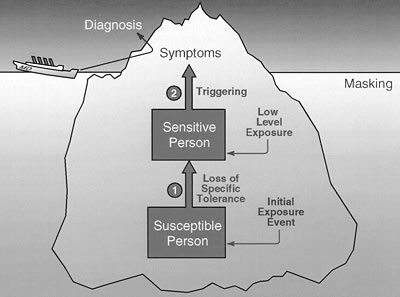
Chemical sensitivity
appears to develop in two stages: Stage 1 – loss of specific tolerance
following acute or chronic exposure to various environmental agents
such as pesticides, solvents, or contaminated air in a sick building;
and Stage 2 – subsequent triggering of symptoms by extremely
small quantities of previously tolerated chemicals, drugs, foods,
and food and drug combinations (e.g., traffic exhaust, fragrances,
caffeine,
alcohol). Physicians formulate a diagnosis based on symptoms reported
to them by their patients. Because of masking, both physicians and
patients may fail to observe that everyday low-level exposures are
triggering symptoms. Sometimes even when such triggers are recognized,
an initial exposure event that initiated loss of specific tolerance
may go unnoticed or may not be linked by the physician or the patient
to the patient's illness.
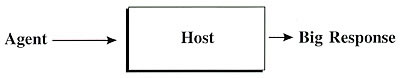
Paracelsus aptly opined that dose makes the poison. However, as our knowledge
has grown, it has become evident that dose + host makes the poison (for example,
pack-years of smoking plus a-1-antitrypsin deficiency). Similarly, in the
case of chemical sensitivity, not everyone exposed in a sick building or
to a chemical
spill develops chronic illness. Thus, it may be concluded that individual
susceptibility, whether physiological or psychological, must play a role
in determining who
gets sick. The term chemical sensitivity fails to convey this key observation
that chemical exposures appear to initiate a process that results in chemical
sensitivity. Conceivably, this phenomenon could represent a new type of toxicity.
The second problem with the term chemical sensitivity is that it suggests
that those afflicted become intolerant of chemical exposures only when
caffeine, alcoholic beverages, various drugs, and foods reportedly trigger
symptoms
in
these individuals, after the process has been initiated.4,12-15 For
the above reasons, chemical sensitivity is a misnomer for the process under
discussion.
An alternative term, toxicant-induced loss of tolerance (TILT), has been
proposed.16 This term offers several advantages. First, it describes the
process as it
has been observed by clinicians and patients. Second, it allows for the
possibility that various toxicants may initiate the process. Third, it
does not limit the
resulting intolerance to chemicals. Finally, it sharpens the focus of the
current debate over chemical sensitivity by positing a theory of disease
that can be
subjected to objective testing.
Historically, new theories of disease arose when physicians observed patterns
of illness that did not fit accepted explanations for disease at that time,
for example, the germ theory or the immune theory of disease. Similarly,
many of the illnesses under discussion here do not conform to current accepted
explanations
for disease or toxicity. Objections to the concept of chemical sensitivity
have included concerns that too many different chemicals have been said to
cause chemical sensitivity; patients report too many symptoms involving any
and every organ system; no known physiological mechanism explains chemical
sensitivity; no biomarker has been identified for chemical sensitivity; and
total avoidance of chemicals is impractical.
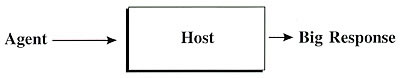
Theories of disease attempt to explain what is going on inside the patient
(a "black box") before overt illness, as illustrated below:
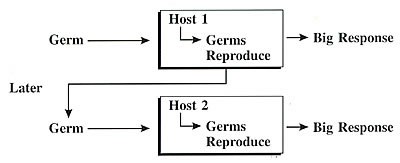
A theory of disease is a yet-to-be-established, general mechanism for a class
or family of diseases. For the germ theory of disease, the boxes depicting
the general mechanism of infection would look something like this:
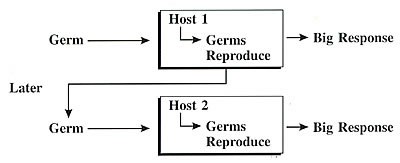
Note
that many different kinds of germs cause responses; there are many
different responses involving any and every organ system (skin,
respiratory, gastrointestinal);
specific mechanisms vary greatly – for example, cholera versus AIDS
versus shingles; there is no single biomarker – identification
of specific germs took years; and prevention (avoidance, antiseptics,
sanitation,
use
of gloves) preceded knowledge of specific mechanisms.
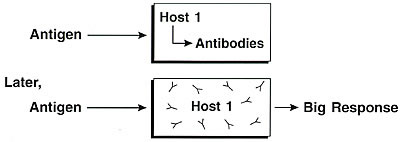
For the immune theory of disease, the boxes might look like this: 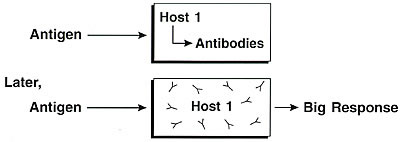
Here, just as for the germ theory
of disease: many different kinds of antigens cause responses; there
are many different responses involving
any and every organ system (skin, respiratory, gastrointestinal); specific
mechanisms vary greatly – for example, poison ivy versus allergic
rhinitis versus serum sickness; there is no single biomarker – identification
of specific antibodies took years; and prevention (avoidance, allergy
shots) preceded knowledge of specific mechanisms.
For toxicant-induced loss of tolerance, the boxes might look like this:
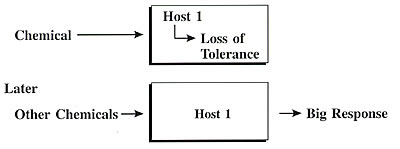
For toxicant-induced loss of tolerance,
as for the germ and immune theories of disease, many different kinds
of chemicals may cause responses;
there may be many different responses involving any and every organ
system; specific mechanisms may vary greatly; it is conceivable that
there is no single biomarker for response – identification of
biomarkers may take years; and prevention (avoidance of initiators
or triggers) may precede knowledge of specific mechanisms.
Although the concept "loss of tolerance" may sound vague,
in fact it is not. What individuals affected report is a loss of specific
tolerance
to particular chemicals, foods, and drugs.16 Note that this theory does not
exclude the possibility that toxicant-induced loss of tolerance could turn
out to be a special kind of toxicity or a variation on the immune theory of
disease, just as allergy and delayed-type hypersensitivity are special cases
that fall under the general classification of immunologic disorders. A consequence
of viewing TILT as a theory of disease would be a shift in perspective from
viewing chemical sensitivity as a syndrome to viewing chemical sensitivity,
now TILT, as a class of disorders parallel to infectious diseases or immunologic
diseases. Much effort has been devoted to developing a case definition for
chemical sensitivity, with a singular lack of success. This lack of success
would not be surprising if in fact TILT represented a new class or family of
disorders. Certainly, it would not be feasible to develop a single clinical
case definition that would embrace all infectious or all immunologic diseases.
Theories of disease that withstand scientific scrutiny arise infrequently.
The past century has witnessed the inculcation of the germ and immune theories
of disease into medical practice. Equating toxicant-induced loss of tolerance
to either one of these theories, both of which have been widely corroborated,
would be premature and presumptuous. On the other hand, toxicant-induced loss
of tolerance has certain earmarks of an emerging theory of disease, including
the vituperative professional disputes that surround it.16
Features of TILT Relevant for Its Testing
As described by many investigators, this phenomenon appears to involve a two-stage
process. Because of ethical considerations, the first stage (initiation)
is more difficult to model in humans than the second stage (triggering).
Ultimately, epidemiologic studies and animal models may elucidate the first
stage. Fortunately, the second stage readily lends itself to testing via
direct human challenges, a potent form of scientific evidence. However, in
the design of human challenge studies in this area, certain key clinical
observations must be taken into account. First, the commonly reported biphasic,
stimulatory-and-withdrawal-like pattern of the patients' symptoms,
particularly those symptoms involving the central nervous system, must be
understood to perform meaningful test challenges on these patients. Second,
a related phenomenon called masking (to be described further) may hide responses
to low-level chemical challenges and therefore may need to be minimized before
testing. Controlling masking may be analogous to controlling background noise
in studies on sound.
The following sections will discuss these clinical features, their incorporation
in experimental designs, and how failure to do so might threaten research outcomes.
Stimulatory and Withdrawal Symptoms
Randolph first described the time course of the responses of these individuals
to chemicals and foods.17 He reported striking parallels between their symptoms
and those associated with alcohol and drug addiction. Randolph viewed the
food and caffeine addictions his patients exhibited as the bottom rungs in
a hierarchy of addiction, proceeding from foods and food and drug combinations
such as caffeine and alcohol on the lower rungs upward to nicotine and other
naturally occurring and synthetically derived drugs.14
Chemically sensitive patients resemble drug addicts in that members of both
groups often report intense cravings and debilitating withdrawal symptoms.
However, chemically sensitive patients' responses are not primarily to
drugs. These individuals more commonly report addictions to caffeine or certain
foods. While drug addicts manifest addicted behaviors (Latin ad "toward" +
dicare "proclaim"), chemically sensitive patients respond as though
they were abdicted (Latin ab "away from" + dicare "proclaim")
and assiduously avoid the very substances addicted persons favor, including
alcohol, drugs, and nicotine.
The stimulatory and withdrawal symptoms reported by chemically sensitive patients
are frequently identical to those reported by normal persons exposed to much
greater amounts of the same substances. For example, after drinking one cup
of coffee, chemically sensitive patients may report feeling hyperactive, jittery,
talkative, nervous, anxious, or experiencing panic-like symptoms (stimulatory
phase). Hours to days later, they may report withdrawal symptoms such as fatigue,
yawning, confusion, indecisiveness, irritability, depression, loss of motivation,
blurred vision, headaches, flu-like symptoms, hot or cold spells, or heaviness
in their arms and legs (withdrawal phase). Similar symptoms occur during caffeine
withdrawal among some low-to-moderate caffeine users in the general population.18
Large numbers of chemically sensitive patients and many Gulf War veterans with
unexplained illnesses report that one drink of an alcoholic beverage causes
inebriation and/or a severe hangover.12,15,19 These augmented responses suggest
that those afflicted have lost their previous natural or native tolerance for
such exposures.
Early in their illnesses, before eliminating caffeine from their diets, many
chemically sensitive patients report having consumed chocolate, coffee, tea,
or cola addictively, often in very large quantities.15 Some carried large containers
of coffee or tea around wherever they went. Many report later stopping use
of all caffeine and xanthines, generally on the advice of a friend or physician,
and subsequently experiencing several days of intense withdrawal symptoms.
Frequently they report that it was only after eliminating all xanthines from
their diets that they were able to discern the effects of consuming a single
cup of coffee or a chocolate bar. Most report becoming aware of the unpleasant
effects of caffeine only after a trial of partial or complete caffeine avoidance.
In this regard, chemically sensitive patients resemble certain reformed smokers
or alcoholics who, after quitting their addictants, report extreme sensitivity
to minute amounts of the addicting agents. Terms like addiction, withdrawal,
and detox pepper the vocabulary of chemically sensitive patients. One patient
described the condition as being "like drug abuse without any of the
fun." These parallels to addiction provide perspective; they may help
explain why the mechanisms that underlie chemical sensitivity have been difficult
to define and why biological markers have proven elusive.
In summary, drug addiction and TILT share a number of features in common. TILT
also has features reminiscent of toxicity and allergy. However, it
is TILT's resemblance to addiction that is perhaps most striking and
that has escaped the attention of many physicians and researchers.
Page 1, 2
|



![]()
![]()